HL7 FHIR - the swagger of healthcare redefining interoperability enabling SMART apps
Work in a medical practice can become so intense, with nearly every spare minute already scheduled for important, pending tasks, that it can sometimes be difficult to see that there are labor-saving options that we simply haven’t yet been able to budget time and resources to investigate.
Since the American Recovery and Reinvestment Act (ARRA) was enacted in 2009, healthcare providers have been forced to switch from paper to electronic health records. There is a universal embrace about health technologies and we all think technology will improve healthcare.
This is how EHR systems came into existence
The EHRs today and challenges
Electronic health record or EHR software is a system that allows medical professionals to quickly enter information on new patients, creating a digital record that they update with each new encounter. The records indicate details including family history, reason for initial complaint, diagnosis and treatment, prescription medications, lab tests, and other vital details needed to provide assistance to each patient.
EHRs have grown in popularity in recent years because they are more convenient to use than antiquated, paper-based records. Practices use them to control access to patient data more securely.
But with technology comes new set of challenges. The healthcare ecosystem is highly complex. It is composed of review boards, regulating bodies, government agencies, pharmaceutical companies, insurance payers, and a mix of public and private provider entities, all of which intersect and overlap. Each party having its own systems and data format. Then there are different EHR systems (EPIC, Cerner and AllScripts to name a few major vendors) that have different tech stack and database structures which poses the challenge of interoperability.
Perhaps the largest problem with Electronic Health Records is the lack of interoperability between disparate systems. To have a full picture of a patient’s medical history, it is important that systems are able to communicate effectively with each other.
Lack of interoperability — one of the biggest downsides of paper record-keeping — has yet to be effectively resolved with electronic record-keeping.
Interoperability and why is it important for Healthcare?
Some of the ambitious projects and missions aiming at establishing a robust and connected Healthcare systems that enable seamless Patient journey and enhanced care. Something that can be made possible when the participants can quickly share and easily interpret the shared data.
India's National Digital Health Mission
"The National Digital Health Mission aims to develop the backbone necessary to support the integrated digital health infrastructure of the country. It will bridge the existing gap amongst different stakeholders of Healthcare ecosystem through digital highways."
Health ID
"Our Health ID is a hassle-free method of accessing your health records digitally. With the ability to create easy to remember HealthID, you can link it with your Aadhaar or Mobile number. Presenting this health ID to a participating healthcare provider will allow you to receive your lab reports, prescriptions and diagnosis digitally from verified doctors and health service providers seamlessly."
MACRA
"Interoperability of health information is a national priority. In the Medicare Access and CHIP Reauthorization Act of 2015, Congress declared it a national objective to achieve widespread exchange of health information through interoperable certified electronic health record (EHR) technology nationwide by December 31, 2018"
21st Century Cures Act
"U.S. healthcare is undergoing a tremendous change. In 2016, Congress passed the 21st Century Cures Act, providing among many things a mandate to end the cycle of patient data being trapped in silos, virtually impossible to share, and keeping the dream or coordinated care out of reach. With the Cures Act came the declaration that US patients should now own their health records and the healthcare industry must make their patient data interoperable, and now the ONC and CMS proposed rules define the terms of compliance and implementation of information blocking provisions in the 21st Century Cures Act, as well as ensuring that patients are able to access their health information."
Five Ways Interoperability Improves Healthcare
Improving patient care and safety is the prime directive and end goal of interoperability. Additional goals are improved care coordination and experiences for patients, lowered healthcare costs, and more robust public health data. How does it accomplish that? Here are the five key benefits of healthcare system interoperability through better information data exchange:
Improved care coordination and patient experiences
Patients must often do administrative tasks like searching for documents, filling out multiple forms, re-explaining their symptoms or medical history and sorting out insurance (both before and, often, after receiving care). This means today’s patient experience is still surprisingly redundant and inefficient. Moreover, the multiple providers who may be providing care for a patient do not have their care coordinated. In fact, the Office of the National Coordinator for Health Information Technology revealed research that shows only 46 percent of hospitals had electronic access at the point of care to the patient information they required from outside providers or sources.
By using interoperability to streamline this process, healthcare facilities will be empowered to give patients faster and more accurate and coordinated treatment, and enhancing their overall experience.
Greater patient safety
According to a study conducted by Johns Hopkins, 44 percent of medical error deaths were preventable. By creating and implementing advanced interoperability, with the aim to capture and interpret data across systems and applications, healthcare organizations can better prevent errors, because of missing or incomplete patient data, and pinpoint their errors’ causes if they do occur.
Even if they have excellent interoperability within their own enterprise, hospitals may be unable to communicate with external affiliates and systems. Lacking data on a patient’s vital signs and history – including allergies, medications or pre-existing conditions — healthcare organizations may be prone to fatal errors.
If care providers can exchange and examine data, they can analyze the exact cause of a medical error to detect the trends in the decision-making leading up to the error. Once a pattern has been identified, healthcare organizations can begin remediating these issues to prevent future errors.
Stronger privacy and security for patients
Patient privacy and security should be a major consideration for any CIO or CISO who is actively looking to improve interoperability within their health system.
Interoperability can help enhance the privacy and security of patient data by requiring organizations to fully assess where their PHI resides and with whom it needs to be shared. When organizations enter data into systems that cannot communicate with one another, for example, it becomes difficult to track all systems that touch PHI, as required by the HIPAA Security Rule. It can be even tougher to track the users with access to an EHR or affiliated applications: In a study of 1 million FairWarning users, 26 percent of users were found to be poorly known or unknown to the care provider.
By promoting interoperability of HR systems such as Lawson or Peoplesoft with your EHR, though, you can better identify users, track their access and more effectively manage access rights. When PHI is entered into secure, interoperable systems, organizations can gain a better idea of where their data is located and who has access to it, helping them secure patient data and protect privacy.
Higher productivity and reduced healthcare costs
According to an estimate from the West Health Institute (WHI), which recently testified in front of the U.S. congress, system interoperability could save the U.S. healthcare system more than $30 billion a year. It can also improve care and hospital safety. Interoperability gives organizations the opportunity to save time with every patient encounter by getting the right data to the patient, the provider and affiliate at the right time, every time.
More accurate public health data
Faster and more accurate collection and interpretation of public health data is possible when IT systems are able to interact. This can help organizations answer pressing questions for both patients and providers. The opioid crisis provides an excellent example of why more robust public health data is needed to understand the scope of that crisis and continue ways to more effectively address and resolve the crisis. By facilitating the sharing and interpretation of such data, interoperability allows healthcare organizations to collectively educate one another on predicting and preventing outbreaks.
SMART on FHIR and the Giant Tech Companies
The goal of SMART is audacious and can be expressed concisely: an innovative app developer can write an app once, and expect that it will run anywhere in the health care system. Further, that app should be readily substitutable for another.”
Kenneth Mandl, MD, MPH
Chair, SMART Advisory Committee
Salesforce
Mulesoft Connectors and Objects corresponding to FHIR based resources in Salesforce Health Cloud

Microsoft
Azure API for FHIR and Entities corresponding to FHIR based resources in Microsoft Health Cloud
Apple
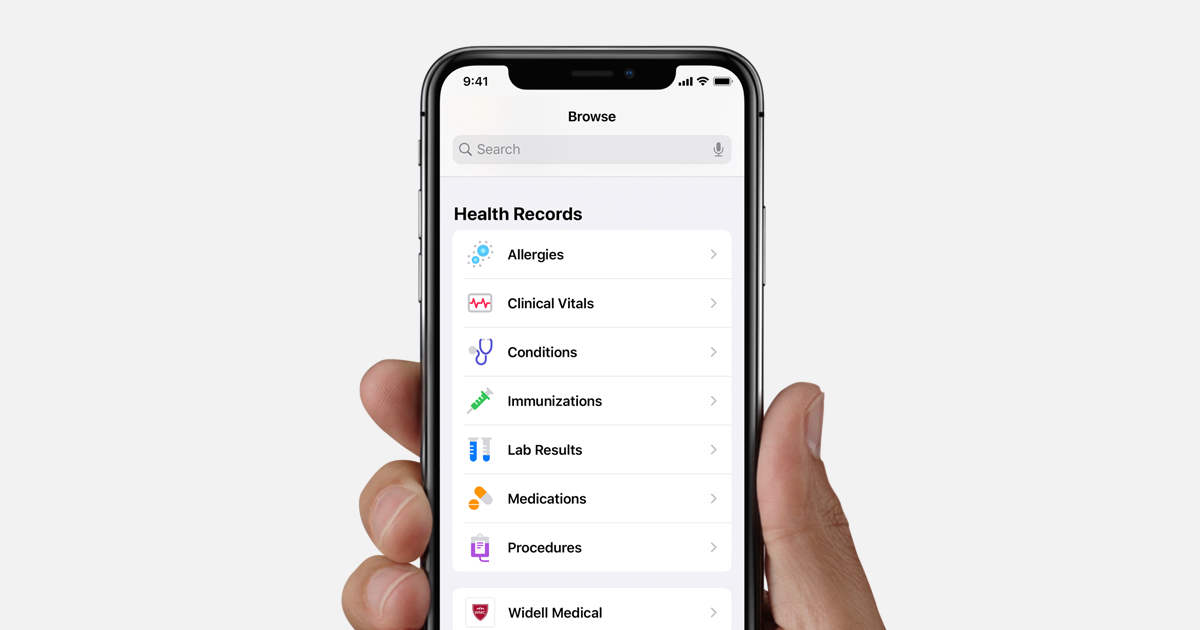
Healthcare APIs
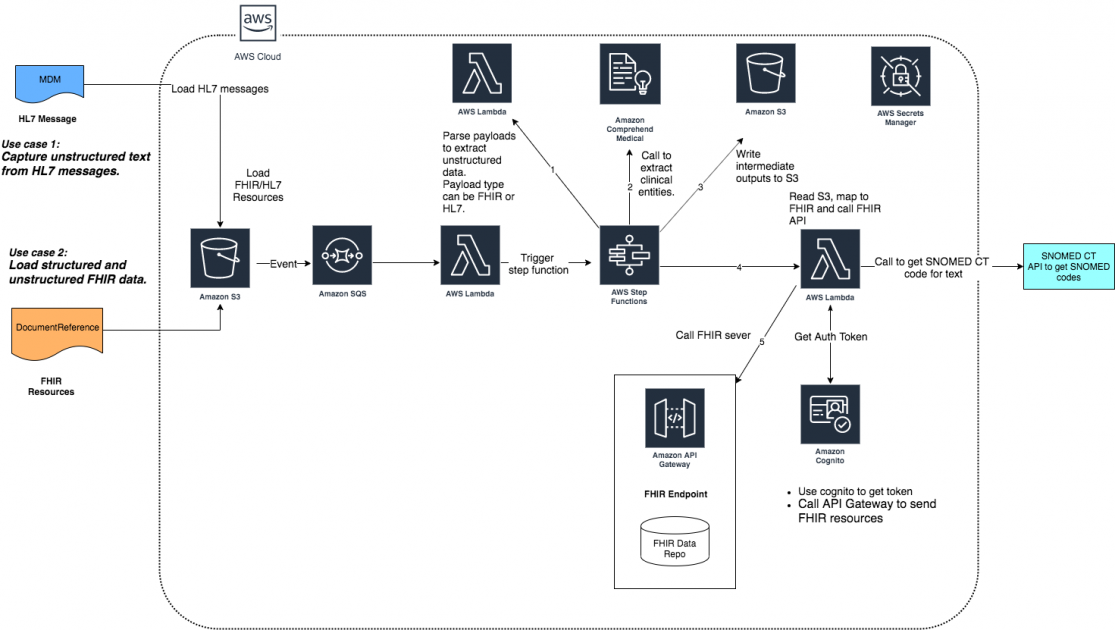
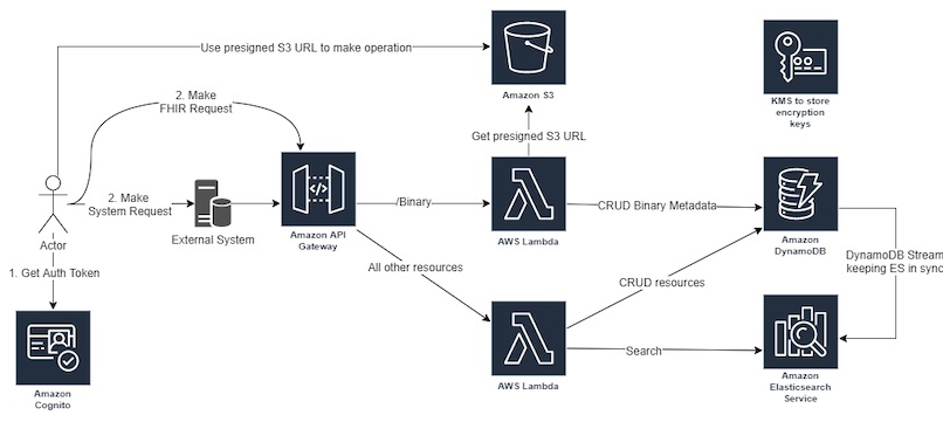
Amazon
What’s Next?
FHIR is an interesting new healthcare standard. It introduces modern web principles to a lagging industry and is authored by an organization that takes the task of defining how clinical data should be structured and exchanged very seriously. What impact FHIR will ultimately have is, like all HL7 Standards, tied to how vendors choose to implement and deploy the standard as well as whether legislation is passed mandating or incentivizing its use.
One thing is clear: We have reached a critical moment in FHIR’s evolution. We are finally starting to see FHIR available in production environments. As developers start interacting with FHIR outside of test environments and start running into the inevitable inconsistencies and quirks associated with something so complex, we will be able to move past the hype to a more informed and measured understanding of the standard. We will stop seeing the articles about how FHIR is going to solve every problem known to healthcare and we will finally be able to assess FHIR for what it is: a tool in the healthcare integrator’s toolbox. Just how useful that tool is and just how often it is the tool of choice remains to be seen
References
https://www.redoxengine.com/wp-content/uploads/2018/07/Redox-on-FHIR_7-18-2.pdf https://www.adsc.com/blog/how-do-ehr-systems-work https://www.beckershospitalreview.com/healthcare-information-technology/the-5-key-benefits-of-healthcare-interoperability.html